Side Menu
|
|
|
 |
|
|
 |
What Are Cataracts?
A cataract is a clouding of the normally clear lens of the eye. The lens, which lies just behind the pupil, helps the eye to focus. When the lens becomes clouded, the passage of light to the back of the eye is partially blocked, and a person's ability to see is reduced. This clouding of the lens of the eye is called a cataract. Thus, a cataract is not a growth or a tumor, but a change in the clarity of the lens. |
| |
Cataracts may form in the eyes of people of any age, but they are most common in older adults. In fact, after age 65, many people have a cataract. It is important to remember that if you have a cataract, you may not necessarily require an operation because many people have some minor clouding of the lens that does not affect vision. An operation to remove the cataract becomes necessary only if the patient's vision and ability to function become impaired. If you do need an operation to remove a cataract, you should know that advances that have been made in cataract operations in recent years have made cataracts one of the most treatable of eye disorders.
Remember, as common as cataract surgery is, no two people undergoing the procedure are alike. The reasons for and the outcome of any operation depend on your overall health, age, the severity of lens opacity (cloudiness), and any other abnormalities of the eye or existing health conditions. |
| |
| Cataract Surgery Techniques |
Extracapsular cataract extraction technique
The surgeon makes an incision where the cornea and sclera meet. Carefully entering the eye through the incision, the surgeon gently opens the front of the capsule and removes the hard center, or nucleus, of the lens. Using a microscopic instrument, the surgeon then suctions out the soft lens cortex, leaving the capsule in place.
|
|
|
| |
Phacoemulsification
Is a modification of the extracapsular cataract extraction. In Phacoemulsification, the nucleus is fragmented by an ultrasonic oscillating probe. The nuclear fragments are simultaneously suctioned from the eye. The size of the incision is smaller than the incision needed to remove the capsule in the extracapsular technique.
An intraocular lens (IOL) is a clear plastic lens that is implanted in the eye during the cataract operation. Lens implants have certain advantages. They usually eliminate or minimize the problems with image size, side vision and depth perception noted by people who wear cataract eyeglasses. They are also more convenient than contact lenses because they remain in the eye and do not have to be removed, cleaned, and reinserted. |
 |
| |
Recovery
You may experience some swelling of the eye area immediately after the operation. If you do, it can be treated with eye drops that contain anti-inflammatory medication. Fortunately, infection is rare after a cataract operation. Nonetheless, an antibiotic ointment or eye drops may be applied directly to the eye for several weeks to ensure that no infection develops.
You should be up and walking soon after the operation. However, you may find that exposure to bright light is uncomfortable. Sunglasses and eye drops can relieve most discomfort you may experience. Your level of activity will depend on your surgeon's instructions. Usually, you can resume normal, non-strenuous activity on the first day after the operation. You also may be asked to wear eyeglasses, both indoors and outdoors, for seven-to-10 days following the operation. In addition, to prevent scratching or irritating the healing wound, you may be asked to sleep with a protective eye shield until the healing process is well under way.
|
 |
| |
Glaucoma isn't one disease. Instead, it's a group of diseases that cause damage to the optic nerve. In most cases, this damage is the result of increased pressure within your eye. As the optic nerve deteriorates, the patient gradually loses the ability to see to the side (peripheral vision). With time your central vision may begin to decrease as well. If Glaucoma isn't treated, it eventually may lead to total blindness.
In fact, Glaucoma is the second most common cause of blindness. That's because Glaucoma often gives no warning sign until permanent damage has already occurred. In most cases the onset is so gradual you're not aware you've lost some of your peripheral vision.
There are several types of Glaucoma, including primary open-angle glaucoma, angle-closure glaucoma, congenital glaucoma and secondary glaucoma. Primary open-angle glaucoma develops slowly and painlessly when normal eye fluid known as aqueous humor doesn't drain properly, causing pressure to build up within your eye. It accounts for 60 percent to 70 percent of all Glaucoma cases.
|
| |
|
|
About 10 percent of people with Glaucoma have angle-closure glaucoma, which occurs suddenly and often causes dramatic symptoms. This type of Glaucoma is a medical emergency and requires immediate treatment. A much smaller number of people have congenital glaucoma, which is present at birth, or secondary glaucoma, which results from trauma, chronic steroid use or disease.
Still, the news about Glaucoma is encouraging. When it's detected and treated early, Glaucoma need not cause blindness or even severe vision loss for most people. |
| |
Signs and Symptoms
The signs and symptoms of Glaucoma vary, depending on the type of Glaucoma. |
| |
Primary open-angle glaucoma
Primary open-angle glaucoma often goes undetected for years. Pressure within the eye increases gradually, with no early warning signs. But eventually, you lose more and more of your side vision until only a narrow section of your visual field remains clear. This type of Glaucoma tends to affect both eyes, although you may have symptoms in just one eye first. In addition to reduced peripheral vision, the signs and symptoms of primary open angle glaucoma may include:
- Sensitivity to glare.
- Trouble differentiating between varying shades of light and dark.
|
| |
Surgery for Glaucoma
When medications aren't effective or well tolerated, surgery may be an option. Keep in mind that surgery doesn't cure Glaucoma. As a result, you may need to keep using antiglaucoma medications even after surgery. In some cases, you may need a second operation.
- Laser surgery (trabeculoplasty). In this procedure, your doctor uses a beam of high energy light to shrink part of the meshwork of your eye's drainage angle. This causes other areas of the meshwork to stretch, which helps aqueous fluid drain more easily. Laser surgery, which usually takes between 10 and 20 minutes, will likely be performed in your doctor's office under local anesthesia. Following surgery you should have almost no discomfort, but you'll need to continue taking eye drops, at least for a time, and you may need more surgery within 5 years. In some cases intraocular pressure actually may increase following laser surgery. In most cases this is temporary, but sometimes the rise in pressure may be permanent, leading to further vision loss.
- Trabeculectomy. In this procedure a surgeon creates a new drainage pathway for fluid in the white part of your eye (sclera) using traditional surgical techniques. Many people who have had this type of surgery no longer need eye drops. But there are also risks. In some cases, scars may form that close the drainage channels. This is a particular problem in young people, blacks and people who have had cataract surgery.
- Drainage implants. This may be an option for adults when other treatments have failed as well as for infants and children. In this procedure a small silicon tube is inserted in your eye to help drain aqueous fluid. Possible complications include the clouding of the lens of your eye (cataracts) and implant failure.
|

|
| |
Angle-closure glaucoma
Attacks of angle-closure glaucoma often develop suddenly, but you also may have preliminary warnings weeks or even months ahead of a severe attack. Glaucoma attacks usually occur in the evening when the light is dim and your pupils are dilated. The pain may be very severe and cause vomiting. Other signs and symptoms of acute glaucoma may include:
- Blurred vision, usually in just the eye involved.
- Halos appearing around lights.
- Reddening of your affected eye.
|
| |
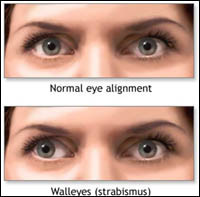
Strabismus is a visual defect in which the eyes are misaligned and point in different directions. One eye may look straight ahead, while the other eye turns inward, outward, upward or downward. You may always notice the misalignment, or it may come and go.
The turned eye may straighten at times and the straight eye may turn. Strabismus is a common condition among children. About 4% of all children in the United States have strabismus. |
| |
| It can also occur later in life. It occurs equally in males and females. Strabismus may run in families. However, many people with strabismus have no relatives with the problem. |
|
|
| |
How Do the Eyes Work Together?
With normal vision, both eyes aim at the same spot. The brain then fuses the two pictures into a single three-dimensional image. This three-dimensional image gives us depth perception. When one eye turns, two different pictures are sent to the brain.
In a young child, the brain learns to ignore the image of the misaligned eye and sees only the image from the straight or better-seeing eye. The child then loses depth perception. Adults who develop strabismus often have double vision because the brain is already trained to receive images from both eyes and cannot ignore the image from the turned eye. |
| |
What Causes Strabismus?
The exact cause of strabismus is not fully understood. Six eye muscles, controlling eye movement, are attached to the outside of each eye. In each eye, two muscles move the eye right or left. The other four muscles move it up or down and at an angle. To line up and focus both eyes on a single target, all of the muscles in each eye must be balanced and working together. In order for the eyes to move together, the muscles in both eyes must be coordinated. The brain controls the eye muscles. Strabismus is especially common among children with disorders that affect the brain, such as:
- Cerebral palsy;
- Down syndrome;
- Hydrocephalus;
- Brain tumors.
What Are the Symptoms of Strabismus?
The main symptom of strabismus is an eye that is not straight. Sometimes children will squint one eye in bright sunlight or tilt their head to use their eyes together.
How Is Strabismus Diagnosed?
Strabismus can be diagnosed during an eye exam. It is recommended that all children have their vision checked by their pediatrician, family doctor or ophthalmologist (medical eye doctor) at or before their fourth birthday. If there is a family history of strabismus or Amblyopia, an ophthalmologist can check vision even earlier than age three. The eyes of infants often seem to be crossed. Young children often have a wide, flat nose and a fold of skin at the inner eyelid that can make the eyes appear crossed. This appearance of strabismus may improve as the child grows. A child will not outgrow true strabismus. An ophthalmologist can usually tell the difference between true and false strabismus.
How Is Strabismus Treated?
Treatment for strabismus works to:
- Preserve vision;
- Straighten the eyes;
- Restore binocular (two-eyed) vision.
After a complete eye examination, an ophthalmologist can recommend appropriate treatment. In some cases, eyeglasses can be prescribed for your child. Other treatments may involve surgery to correct the unbalanced eye muscles or to remove a cataract. Covering or patching the b eye to improve Amblyopia is often necessary. |
| |
|
The cornea is the front window to the eye. It allows light into the eye and bends (refracts) the light rays to help the lens focus them upon the retina. To perform properly, the cornea must be crystal clear and be a proper curvature.
What Causes the Cornea to Become Cloudy?
There are many causes for the clouding for the cornea. They include the following: |
|
 |
- Eye injuries that leave a dense white scar on the cornea. These injuries may include penetrating wounds from a sharp object, burns, or chemical contamination of the eye.
- A severe corneal infection that leads to corneal scarring. The infection may be bacterial, viral, or fungal in origin. Various herpes viruses are known to cause such scarring.
- Abnormal shapes of the cornea, caused by diseases such as keratoconus, may scar the center of the cornea or distort vision so severely that glasses or contact lenses are of little help.
- Corneal dystrophies may cause clouding.
- Inherited diseases of the cornea
- Cataract or other eye surgery can prompt corneal clouding.
Where Does Corneal Transplant Tissue Come From?
During corneal transplant surgery, only the clear, central part of the cornea is replaced. Corneal tissue used for transplant surgery comes from donors. An eye bank procures the tissue, examines it, and then stores and protects it until used. All tissue used for transplantation is extensively tested. It is screened for the presence of communicable diseases such as hepatitis and the presence of HIV (the AIDS virus).
How is a Corneal Transplant Performed?
The corneal transplant operation may be performed under either a local or general anesthetic, depending on what the doctor believes to be in the patient's best interests. The surgeon removes the center of the cloudy cornea and replaces it with the clear donor cornea. The donor tissue is sewed in place.
If a cataract is present the surgeon can remove it as part of the corneal transplant operation. If an artificial lens is already in place in the eye and it is believed to be responsible for the clouding of the cornea, the artificial lens can be replaced with a type of lens less likely to irritate the donor corneal tissue.
 What Happens After A Corneal Transplant Operation? What Happens After A Corneal Transplant Operation?
The eye is patched overnight and examined the next day. Usually, there is little or no discomfort after surgery. In most cases, resumption of normal activities may occur soon after surgery with some reasonable limitations. For example, lifting heavy objects or strenuous exercise must be avoided until directed otherwise by the physician.
Until the eye has healed, glasses or an eye shield must be worn to protect the eye. For several weeks following the transplant surgery, eye drops will be prescribed. The eye drops are to prevent infection and rejection of the donor corneal tissue.
The sutures used to sew the donor cornea in place are barely visible and do not cause pain. It is normal for the eye to feel scratchy or irritated for the first few days following surgery. As the cornea heals, some of the stitches used to sew the donor tissue into place are removed. This can be done quite easily in the doctor's office. During the first few weeks after surgery, vision is usually quite blurry. It takes time for the eye to completely heal after surgery. It may take four to six months or even longer for the cornea to stabilize. Once the cornea stabilizes, improved vision is usually enjoyed. Glasses or contact lenses may be required. In some cases, Astigmatism may be noticeable. Often, this can be corrected with glasses or contact lenses.
What Are The Risks Of Corneal Transplant Surgery?
Just as is true with any operation, corneal transplant surgery entails some degree of risk. The success of the transplantation surgery is often related to the original cause of the underlying corneal disease process.
Transplant procedures resulting from abnormally shaped corneas due to keratoconus or for corneal clouding following cataract surgery typically have very high success rates. Conversely, transplants due to scarring of the cornea from infections, such as herpes, typically have a lower success rate.
Rejection of the transplanted tissue can occur following corneal transplant surgery. Corneal graft rejection rarely occurs within 2 weeks and may occur as late as 20 years following corneal transplant. Pain, light sensitivity, redness, and decreasing vision are warning signs of corneal tissue rejection and indicate the need for immediate medical attention. When started at the first signs of tissue rejection, steroids (drops, injections, and/or pills) may be effective in halting the rejection process.
If the rejection process continues, the donor tissue becomes cloudy, resulting in blurry vision. Often, a repeat transplant may be performed.
The risk always exists that vision could be permanently impaired or lost. Other possible complications include bleeding, infection, scarring, glaucoma, retinal swelling, retinal detachment, cataract formation, and swelling of the donor graft.
Although risks are present, the success rate of corneal transplantation is very high. It enjoys the highest success rate of any transplant procedures commonly performed. |
| |
Every year, one hundred thousand men and women choose Blepharoplasty to improve the way they look. Droopy eyelids can make you look older and can also impair vision. Blepharoplasty corrects these problems and also removes puffiness and bags under the eyes that make you look worn and tired.
This procedure cannot alter dark circles, fine lines and wrinkles around the eyes, nor can it change sagging eyebrows.
Though Blepharoplasty is often performed as a single procedure, your surgeon may also recommend a brow lift, facelift, or skin resurfacing to achieve the best results.
If you are wondering how Blepharoplasty can change the way you look, you need to know how eyelid surgery is performed and what you can expect from this procedure. This pamphlet can address many common questions and provide you the information to begin considering Blepharoplasty. |
|
 |
| |
| Successful facial plastic surgery is a result of good rapport between patient and surgeon. Trust, based on realistic expectations and exacting medical expertise, develops in the consulting stages before surgery. Your surgeon can answer specific questions about your specific needs. |
| |
| Is Blepharoplasty for you? |
| As with all facial plastic surgery, good health and realistic expectations are prerequisites. Blepharoplasty removes the excess fat, muscle, and skin from both upper and lower lids. The results can be a refreshed appearance, with a younger, firmer eye area. |
| |
People with circulatory, ophthalmological, or serious medical conditions must rely on the diagnostic skills of their own personal specialists to determine whether Blepharoplasty is an option to consider. Consultation with the facial plastic surgeon can help you decide whether any additional, complementary surgery would increase the success of the surgery. Your surgeon might recommend planning a simultaneous forehead lift to correct a drooping brow and smooth the forehead, or skin resurfacing to remove the fine line wrinkling in the eye area.
Making the decision for Blepharoplasty whether the surgery is desired for functional or cosmetic reasons, your choice of a qualified facial plastic surgeon is of paramount importance. The patient must also make the commitment to follow the pre-surgical and post-operative instructions of the surgeon. |
| |
During the pre-surgical consultation, you will be examined or asked to answer queries concerning vision, tear production, use of lenses, and your desires for surgery. Your surgeon will explain what you can expect from Blepharoplasty and take a complete medical history. Factors to be weighed include age, skin type, ethnic background, and degree of vision obstruction. Furthermore, you can expect an open and honest exchange between you and your surgeon, which will establish the basis for a successful outcome.
After both you and your surgeon make a mutual decision, the technique indicated for your individual surgery will be discussed. The type of anesthesia, the surgical facility, any supportive surgery, and the risks and costs inherent in the procedure will be outlined. |
| |
Understanding the Surgery
In upper eyelid surgery, the surgeon first marks the individual lines and creases of the lids in order to keep the scars as invisible as possible along these natural folds. The incision is made, and excess fat, muscle, and loose skin are removed. Fine sutures are used to close the incisions, thereby minimizing the visibility of any scar.
In lower eyelid surgery, the surgeon makes the incision in an inconspicuous site along the lash line and smile creases of the lower lid. Excess fat, muscle, and skin are then trimmed away before the incision is closed with fine sutures. Eyelid puffiness caused primarily by excess fat may be corrected by a transconjunctival Blepharoplasty. |
| |
The incision in this case is made inside the lower eyelid, and excess fatty material is removed. When sutures are used to close this kind of incision, they are invisible to the eye. They are also self-dissolving and leave no visible scar. Under normal conditions, Blepharoplasty can take from one to two hours.
What to expect after the surgery
Immediately after the surgery has been completed, your surgeon may apply tiny sterile bandages. This is not done for transconjunctival Blepharoplasty. It is not crucial that the eyes be covered. However, an ointment to prevent dryness of the eye area may be used. A certain degree of swelling and bruising is normal. Cold compresses, as well as head elevation when lying down, will enhance healing and relieve discomfort. Your surgeon will prescribe medication for discomfort.
For a week and a half following Blepharoplasty, you will clean the eye area (the eyes may feel sticky, dry, and itchy). Eye drops may be recommended. Your surgeon will also list activities and environments to avoid in the weeks immediately following surgery. Permanent stitches will be removed in three to five days after surgery. Self-absorbing stitches will dissolve on their own.
Facial plastic surgery makes it possible to correct many facial flaws and signs of premature aging that can undermine self-confidence. By changing how you look, facial plastic surgery can help change how you feel about yourself.
Insurance does not generally cover surgery that is done purely for cosmetic reasons. Surgery to correct or improve vision or surgery for eye deformity or injury may be reimbursable in whole or in part. It is the patient's responsibility to check with the insurance carrier for information on the degree of coverage. |
| |
What is a Keratoconus?
The normal cornea usually has a spherical curvature. A disease called keratoconus causes the cornea to undergo progressive thinning and thus protrude outward, forming a cone-like curvature, which leads to distortion and decreased vision. The disease is thought to be inherited and begins to manifest itself sometime in the late-teen through early adult years.
Treatment for Keratoconus
In some cases, glasses or contact lenses may improve vision in patients with keratoconus. More severe cases may require removal of the affected cornea and replacement with donor tissue through a cornea transplant operation.
|
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
| |
|
 |
|
|
|
|
|




 عربي
عربي





















 What Happens After A Corneal Transplant Operation?
What Happens After A Corneal Transplant Operation? 